The role of AI in medical EHR in 2026 is no longer a “someday” topic. It already affects how you document care, how you find critical facts, and how you move patients through the system without missing details. Yet 2026 raises the bar. You cannot rely on extra clicks, extra screens, and extra memory. You need the EHR to behave like a smart assistant that stays grounded in the chart.
You probably feel the pressure from both sides. On one side, patients expect quick answers and cleaner continuity. On the other side, teams face heavy loads, complex compliance rules, and constant handoffs. So, you need tools that cut noise without cutting safety. That is exactly where AI and EHR starts to matter in a practical way.
If you’re mapping an EHR roadmap for 2026, this guide on EHR Software Development From The Ground Up explains what modern platforms need before AI gets layered in.
AI Integration In Electronic Health Records Becomes Native In 2026 (Not An Add-On)
In the past, AI often lived outside the EHR. You exported data, used a separate product, and then copied the results back. That broke the flow. It also made teams distrust the output. In 2026, the winning pattern looks different: AI integration in electronic health records becomes native. It sits on the same screen where you click orders, write notes, and review labs.
This shift does not happen by accident. Vendors now push AI roadmaps as core EHR strategy. Oracle, for instance, announced an AI-driven EHR direction in August 2025 and said it planned to add a “full spectrum” of acute care functionality in 2026.
That statement matters because acute care raises the stakes. It forces AI features to operate under tighter clinical, operational, and documentation demands. In other words, 2026 expects AI-powered electronic health records to work where timing, coordination, and accuracy matter most.
The Role of AI in Summarizing Medical Records
Medical records summaries are critical in patient care, legal proceedings, insurance claims, and overall healthcare operations. They condense complex patient information into coherent and concise summaries, providing an overview of key medical events, treatments, surgeries, and other essential data.
Over the past two decades, medical document summarization has been a common practice, but creating such summaries has traditionally been time-consuming and prone to human error.
However, AI and NLP are now revolutionizing this process. AI technologies, powered by machine learning and Natural Language Processing (NLP) techniques, have transformed how medical records are analyzed and summarized.
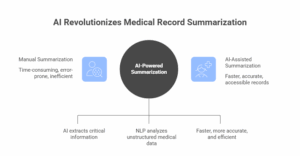
Through advanced data processing and optical character recognition, AI algorithms can extract critical information from vast amounts of unstructured medical data, making the medical records summary creation process faster, more accurate, and more efficient. This not only saves valuable time but also enhances the accessibility and usability of medical records, benefiting patients, healthcare providers, and other stakeholders.
What “EHR AI” Means When You Look Under The Hood
People toss around EHR AI as if it were a single feature. It is not. It is a stack of capabilities that work together. When the stack works, you get speed plus confidence. When it fails, you get polished text that you cannot trust.
At a high level, AI in electronic medical records usually works through five layers:
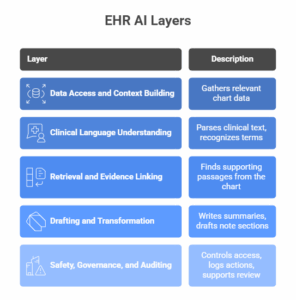
This structure explains something important: generation is not the first step. Retrieval and grounding matter first. That is why mature AI tools’ electronic health records optimization work tends to start with “find the truth in the chart,” then move to “write a draft you can approve.”
If you’re planning architecture and vendor comparisons, AI Tech Stack lays out the components that make retrieval, grounding, and controlled drafting work in production.
How AI Fits Into The EHR In 2026: Three Common Patterns
In 2026, AI and electronic health records tools tend to appear in predictable spots. These spots map to where people lose time.
| Workflow Area | What AI Does In 2026 | What You Should Demand |
| Documentation | Drafts structured content, supports ambient capture, and cleans formatting | Clear source grounding and easy editing before signing |
| Chart Review | Builds timeline views and AI medical records summary outputs | Evidence links to notes, labs, and scanned records |
| Inbox And Coordination | Drafts messages, routes tasks, and reduces context switching | Safe templates, strict review steps, and role-based controls |
This table looks simple, yet it highlights a key truth: AI succeeds when it reduces switching and scrolling. It fails when it forces you into a separate tool or produces text you cannot verify.
Many teams ask a simple question: “Does AI actually save time in the EHR?” A strong 2025 pre–post study using Epic “Signal” metrics offers a concrete answer with EHR-native measurement. The study found rapid uptake of an ambient tool and measurable time savings:
Adoption rose from 15% to 50% in 8 weeks. Mean time in notes per note dropped from 5.11 to 4.16 minutes (0.95 minutes saved per note, 18.6% reduction).
This stat matters because it is not hand-wavy. It uses operational EHR metrics. It also reflects real behavior change over a short period. So, in 2026, you should expect more organizations to measure AI impact using system telemetry, not only surveys.
Key Applications Of AI In EHR Workflows In 2026
This section goes deeper. It explains how AI applications in electronic health records show up in real environments, not just in product brochures.
Documentation: From Typing To Editing
Documentation remains at the front door. When documentation gets easier, everything downstream gets easier too: coding, coordination, referrals, and follow-up instructions.
In 2026, modern documentation tools focus on these steps:
- Capture the encounter (voice, structured inputs, and existing chart context)
- Draft a note in your preferred structure
- Let you edit quickly, then sign
You should see AI in electronic health records reduce “blank page time.” That is the time spent staring at an empty template, hunting facts, and deciding how to start.
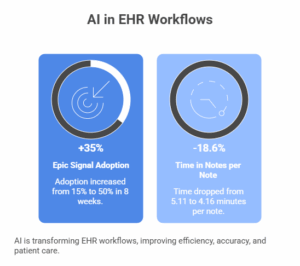
The Epic “Signal” pre–post study supports this direction with specific measurements tied to note-writing time. Adoption moved from 15% to 50% in 8 weeks, while time in notes per note dropped from 5.11 to 4.16 minutes, saving 0.95 minutes per note and reducing time by 18.6%.
That does not mean every tool performs the same. Some tools create long drafts that slow review. Others push short, structured drafts that fit real practice. In 2026, you should prioritize tools that respect your structure and reduce cognitive load during edits.
Chart Summaries: Making The Record Read Like A Story
A chart should tell a story. Instead, it often reads like a pile of fragments. That is why AI medical records tools gain traction in chart review.
In 2026, chart summarization improves when it moves away from one giant paragraph. You want a set of views that match how you think:
- A problem-focused summary
- A timeline of key events
- A medication change history
- A diagnostic trend view
- A contradictions panel (allergy conflicts, duplicate meds, mismatched problem lists)
This is where the phrase AI medical records summary should mean something concrete. It should mean: “You can verify facts in seconds.” It should not mean: “You got a pretty narrative with no evidence trail.”
Also, summarization supports handoffs. It supports consults. It supports triage. It supports discharge planning. So, it becomes a broad multiplier across care settings.
Retrieval: Finding The Right Fact At The Right Time
Chart retrieval sounds basic. Yet it drives most daily frustration. If you cannot find the last colonoscopy result or the last anticoagulation plan, you waste time. Worse, you risk missing key decisions.
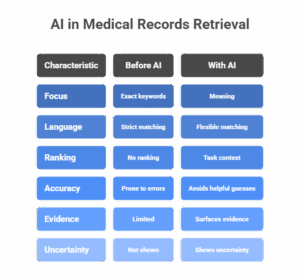
In 2026, AI in medical records retrieval focuses on meaning rather than exact keywords. It pulls relevant snippets even if the language varies. It also ranks results based on task context.
For example, a retrieval system may treat these as related: “heart,” “MI,” and “myocardial infarction.” That simple mapping saves time because you do not need to guess which term someone used in a prior note.
However, retrieval must avoid the trap of “helpful guesses.” It should not fill gaps with invented facts. It should surface evidence and show uncertainty when evidence is missing.
Coding And Documentation Integrity: Reducing Denials Without Overreach
Coding support sits at the intersection of clinical documentation and reimbursement. In 2026, the best systems focus on integrity, not aggressive automation.
Expect these patterns:
- AI flags missing documentation that payers often challenge
- AI suggests where a diagnosis needs clearer support
- AI highlights mismatches between assessment and plan
- AI helps build consistent narratives for prior authorization
This is one of the most pragmatic uses of AI and EHR because it cuts loops between clinicians and billing teams. Still, you should keep control tight. You want suggestions that link back to documentation. You also want transparent logs for audit readiness.
Patient Communication: Drafting That Keeps You In Control
Patient messages keep rising. So, AI in electronic health records increasingly supports message drafting.
In 2026, you should see message AI behave like this:
- It reads the patient’s question
- It pulls relevant chart facts (meds, allergies, recent labs)
- It drafts a clear reply in plain language
- It prompts you to review, edit, and send
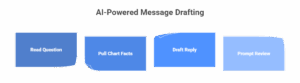
This workflow works because you stay in control. It also reduces the time spent rewriting the same explanations.
However, safe tools must avoid clinical overreach. They should not diagnose through the portal. They should not downplay urgent symptoms. They should prompt escalation when needed.
Acute Care Expansion: Why It Signals Maturity
Acute care adds complexity: orders, rapid changes, handoffs, and intense documentation. That is why Oracle’s August 2025 announcement matters. It explicitly referenced an AI-driven direction and planned acute care expansion in 2026.
When AI features support acute workflows, they can often support other settings as well. Still, acute care also increases scrutiny. In 2026, you should expect stronger governance, tighter audit trails, and stricter deployment rules.
Benefits For Healthcare Providers And Patients In 2026
Benefits sound easy to list. Yet the real value sits in specific daily moments. So, this section stays grounded in what changes minute by minute.
For providers, AI-powered electronic health records can reduce:
- Time spent searching across tabs
- Time spent formatting notes
- Time spent rewriting the same medical history
- Time lost to unclear handoffs and repeated questions
For patients, AI and electronic health records can improve:
- Continuity across visits
- Clarity of instructions and follow-up plans
- Speed of responses when teams use draft-and-review messages
- Consistency when multiple clinicians share a patient
Still, these benefits only appear when systems enforce verification. Patients do not benefit from faster errors. Providers do not benefit from faster chart noise. So the best 2026 deployments treat AI as “draft plus evidence,” not “auto-post.”
Benefits For Legal And Insurance Professionals
Legal and insurance workflows require clear chronologies, defensible facts, and repeatable review steps. They also require strict compliance with the handling of PHI and record access.
In 2026, AI medical records tools will help most when they focus on structure:
- Convert scattered notes into a timeline with dates and sources
- Identify gaps where records appear to be missing
- Extract key events like admissions, procedures, and follow-up instructions
- Reduce review time by making records searchable by meaning
This is also where AI in medical records retrieval changes the experience. Instead of manual scanning, you can retrieve relevant passages tied to a claim question. Yet you still need verification. A legal summary that cannot point to source pages creates risk.
So the best tools combine structured extraction with strong evidence trails. They also keep logs that show who accessed what, when, and why.
How AI Works in Medical Records Summarization
The healthcare industry has been using AI for some time for tasks like adverse event prediction and optimizing operating room scheduling. Still, the sector has $1 trillion worth of untapped improvement potential, and AI is a significant new instrument that can help unlock some of it.
AI-driven medical records summarization is a technological breakthrough that leverages the capabilities of artificial intelligence and natural language processing (NLP) to automate the extraction and summarization of relevant information from medical records. This innovative approach aims to enhance the efficiency of medical record review and analysis while ensuring accuracy and completeness.
- Optical character recognition (OCR)
AI systems use OCR technology to convert scanned or handwritten medical records into machine-readable text, overcoming the limitations of traditional document formats. - NLP algorithms
Natural language processing algorithms enable AI systems to understand the context, relationships, and nuances within medical records. These algorithms analyze the language used in medical documents, extracting key information and identifying relevant patterns. - Generative AI
Modern large language models allow for creating human-like summaries by generating coherent and contextually relevant text. This goes beyond simple keyword extraction, ensuring a nuanced understanding of the content. - Chronological medical record indexing.
AI systems can automatically create a chronological index of events and treatments, providing a clear timeline of a patient’s medical history. This feature is particularly valuable for legal professionals and clinicians seeking a concise overview.
Challenges And The Future Of EHR AI In 2026
Every big shift creates new risks. In 2026, the hardest problems sit in trust, governance, and data quality.
Here are the core issues, explained without scare tactics.
| Issue | Description | Risks / Consequences | Recommended Actions |
| Hallucinated details | The model may confidently claim a fact that the chart does not support. | Misinformation, loss of trust, and potential reporting errors. | Implement evidence linking, use “unknown” flags, and ensure traceable data sources. |
| Chart messiness | Duplicate entries, outdated problem lists, and copy-forward artifacts complicate summarization. | Reduced AI accuracy, error propagation, and team confusion. | Establish regular data cleanup, reconciliation routines, and charting standards. |
| Workflow drift | Teams may stop verifying system drafts over time. | Increased risk of errors, decline in quality control. | Define clear review checkpoints, implement validation protocols, and support audit trails. |
| Privacy controls | AI tools handle sensitive or personal data. | Data breaches, GDPR/HIPAA non-compliance, and reputational damage. | Apply role-based access, log all actions, and enforce secure data retention and deletion policies. |
| Integration fragility | AI features often rely on APIs and EHR UI hooks, which can be unstable. | Service interruptions, data sync failures, and dependency on vendors. | Develop stable integration plans, include monitoring tools, and maintain vendor accountability through SLAs. |
In 2026, the future belongs to systems that treat AI as a governed workflow, not a magical text engine. That is how AI-enhanced electronic health records market offerings separate serious platforms from “feature lists.”
What To Look For When Evaluating AI EHR Tools In 2026
This section stays practical. It focuses on what you can test in demos and pilots.
If a tool cannot show evidence for key claims, it should not draft clinical facts. If a tool cannot handle outside documents, it should not promise complete summaries. If a tool cannot log actions, it should not operate at scale.
| Evaluation Area | Good Signal In 2026 | Bad Signal In 2026 |
| Evidence | Output links directly to source notes, labs, or scanned pages | Output reads well, but cannot show where the facts came from |
| Workflow Fit | Drafts match your templates and shorten editing time | Drafts create extra review work or awkward formatting |
| Governance | Strong logs, access controls, and clear review steps | Vague controls, weak auditing, unclear retention policies |
This table helps you quickly screen tools. It also aligns with how compliance and clinical leadership think during the adoption process.
How “AI Medical Records” Tools Should Handle Scanned And Outside Data
Scanned documents still drive many review headaches. They arrive as PDFs, faxes, or uploaded images. They often contain key context. Yet they remain hard to search and harder to summarize.
In 2026, AI in medical records retrieval should handle this pipeline:
- Identify document type (discharge summary, consult note, imaging report)
- Extract sections (impression, plan, meds, diagnoses)
- Normalize key entities (conditions, procedures, medication names)
- Place events on a timeline with dates and confidence markers
When that pipeline works, you stop missing important outside facts. You also reduce duplicate testing. That helps both clinical outcomes and cost control.
This area is also important for legal and insurance review, as many case files include scanned material. If AI cannot parse those documents, it cannot give complete summaries.
The Human Side: Adoption, Training, And Trust In 2026
Technology does not fail only due to software. It fails because people do not trust it or do not know how to use it safely.
In 2026, adoption improves when training focuses on editing and verification rather than “prompt tricks.” People need routines:
- Verify the top facts first
- Confirm meds, allergies, and recent labs
- Shorten drafts without losing key details
- Correct errors and feed feedback into governance
Also, leaders should set the expectation that AI drafts do not equal final documentation. Review remains part of the workflow. That mindset keeps quality stable even when speed increases.
Finally, teams need a style guide. Without it, AI output varies too much. With it, the draft becomes predictable, and clinicians feel less friction.
These tables aim to be copy-friendly for internal training documents.
| Task | Best AI Assist Pattern | What You Verify First |
| Follow-up visit note | Draft HPI + assessment from last visit and new labs | Changes since last visit and red-flag symptoms |
| Consult request | Create a clean timeline summary for the specialist | Diagnosis history and key diagnostic results |
| Prior auth narrative | Draft structured justification tied to chart facts | Indication, failed alternatives, and documentation alignment |
These patterns keep AI grounded in real work and reduce wasted effort.
If you’re scaling fast and need extra engineering support, Outsource Healthcare Software Development explains what to delegate, what to keep internal, and how to control risk.
2026 EHR AI Governance: Privacy, Audit Trails, And “Source-First” Trust
In 2026, the biggest upgrade in AI and EHR is not a new model. It is the way you control the model inside the clinical record. If you want AI-powered electronic health records to work in real settings, you need rules that match how risk shows up in daily care. That starts with one principle: every output must stay tied to the chart.
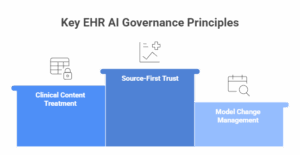
A draft note, a chart summary, or a coding suggestion should never float as “model opinion.” It should point back to the exact note, lab, or document that supports it. This is how using AI to improve electronic health records stays safe when pressure rises.
Governance also means treating generated text like clinical content, not like a chat response. You need a clear approval chain, you need role-based access, and you need logs. Logs matter because they answer tough questions later: who generated what, what sources were used, who edited it, and who signed it. Without this, AI in electronic health records can increase liability, even if it saves time.
Another 2026 issue is model change. Vendors update models. Prompts change. Interfaces change. That can shift behavior overnight. So you should require release notes, test windows, and rollback options. You should also run periodic “chart truth” checks: pick real cases, compare AI summaries against source documents, and track errors like missing diagnoses, wrong dates, or medication mix-ups. This is especially important for AI in medical records retrieval, because one retrieval mistake can poison every downstream draft.
Final Thoughts
In 2026, you can treat AI as a sidebar tool, or you can treat it as a workflow layer that reduces friction across documentation, chart review, and retrieval. The second approach wins because it respects how care actually happens: fast decisions, limited time, and heavy coordination. That is why the role of AI in Medical EHR in 2026 belongs in your EHR roadmap now, not later.
We at LITSLINK have strong experience in Custom Software Development and healthcare-grade solutions. We can build secure AI features that fit EHR workflows, keep evidence trails, and support governance from day one. Contact LITSLINK and let’s get started.





